Child
- About
- Meet The Team
- Conditions
- Aortic Stenosis
- Atrial Septal Defect
- Coarctation of the Aorta
- Complete Atrioventricular Septal Defect
- Heart Murmur
- Interrupted Aortic Arch
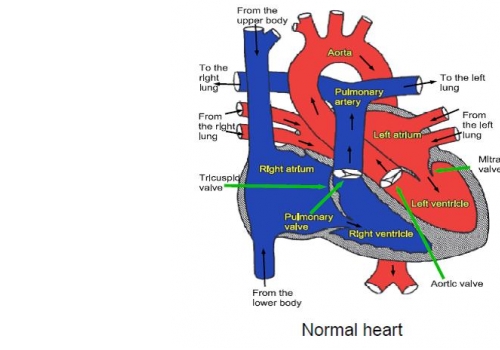
- Normal Heart
- Partial Atrio-Ventricular Septal Defect
- Patent Ductus Arteriosus
- Pulmonary Atresia with Intact Ventricular Septum
- Pulmonary Atresia with Ventricular Septal Defect
- Pulmonary Stenosis
- Right Aortic Arch
- Small Ventricular Septal Defect (Muscular)
- Small Ventricular Septal Defect (Perimembraneous)
- Tetralogy of Fallot
- Transposition of the Great Arteries
- Ventricular Septal Defect (Large)
- Dental Practitioners: Dental care in children at risk of Infective Endocarditis
- Looking after your child’s oral health
- Coming for an echocardiogram
- Outpatient Appointments
- Preparing to Come into Hospital for Surgery
- On Admission to the Children's Ward
- Visiting
- Operation Day
- Children's Intensive Care
- Daily Routine on Intensive Care
- Managing your child's discomfort
- Going Home
- Children's Cardiac MRI Scan
- Cardiac Catheter
- Reveal Device
- Ablation Procedure
- Pacemakers
- INR and Warfarin
- Lifestyle and Exercise Advice
- School Advice
- Attachment
- Yorkshire Regional Genetic Service
- Advice & Support Groups
- Your Views
- Monitoring of Results
- Second Opinion
Pulmonary Atresia with Ventricular Septal Defect
This is a serious heart condition in which there are two main abnormalities:
- the artery which normally allows blood to be pumped from the heart to the lungs (the pulmonary artery) is completely blocked
- there is a large hole (ventricular septal defect) between the two main pumping chambers (ventricles) of the heart.
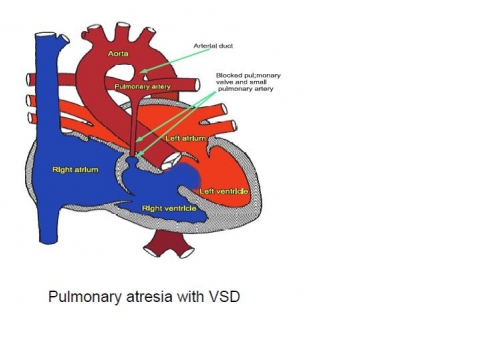
In the normal circulation, blood passes through the lungs to collect oxygen from the air. In babies with pulmonary atresia less blood passes through the lungs and this reduces the amount of oxygen in the blood. This makes the baby (particularly the lips and hands) appear blue, and if the body becomes very short of oxygen the baby will die.
Before babies are born the two main arteries arising from the heart (one called the aorta, which feeds the body with blood and one called the pulmonary artery, which feeds the lungs with blood) are joined together by a short blood vessel called the arterial duct (often just called the duct). Most babies with pulmonary atresia appear well for a while because the duct allows the lungs to be supplied with blood from the aorta.
In normal babies the duct closes off by itself shortly after birth because it is no longer needed, but if the duct closes in a baby with pulmonary atresia the baby will become very blue and will die because no blood can get to the lungs. The duct can usually be prevented from closing by giving the baby a drug called prostin. Most babies with pulmonary atresia will need an operation within the first few weeks of life to make sure they can feed their lungs with blood. This operation involves connecting the artery leading to one of the arms to the artery which leads to the lungs, and is called a “shunt” operation. This doesn’t make the baby’s heart normal, but it usually allows the baby to survive until he or she is old enough to consider more major surgery.
Even major surgery later in life cannot make the heart completely normal and it is very unlikely that any child with pulmonary atresia and VSD will have a normal lifespan
Tests
Tests such as an ultrasound scan of the heart (an “echo”), and an x-ray of the chest are required, although some babies will need more complicated x-ray tests (called a cardiac catheterisation or CT scan).
Other abnormalities
Some babies with pulmonary atresia and VSD will have other abnormalities. The commonest of these is a genetic abnormality, where a small part of one chromosome is missing. This abnormality is called “22q11 deletion” or Di-George Syndrome. Although some children with Di-George syndrome grow and develop normally, some will have learning or speech difficulties and if your baby has Di-George Syndrome, it is important that his or her development is monitored so that help can be given early if necessary. A blood test to check for this abnormality is usually done, but it may take some weeks for the result to come back.
The shunt operation
All heart operations in babies are serious and will carry some risk of the baby dying or having major complications such as brain damage, kidney damage or lung complications such as pneumonia. For shunt operations the risk of a baby dying is small (about 2 in 100) and the risk of brain damage is also small (probably around 1 in 100). These risks are higher if the baby has other abnormalities or if the baby has been born prematurely.
Further surgery when the baby has grown
All children with pulmonary atresia and VSD who have had a shunt operation as a baby will need further treatment when they are older. Exactly what this treatment will be depends very much on how the baby grows. One of the most important factors is how well the pulmonary arteries grow. If they grow well it may be possible, with major surgery, to open up the blockage between the heart and the pulmonary artery (sometimes using a human or pig’s valve) and to close the ventricular septal defect by sewing a patch over it. This is often referred to as “corrective” surgery, but it does not make the heart completely normal. Human or pig valves may become narrow as they age and it is possible that further treatment will be needed.
Even many years after apparently successful surgery new problems may arise which require treatment. One of the late problems is the development of abnormal heart rhythms. These can usually be treated, but can be serious and can even rarely be fatal, so regular review in outpatients by a specialist is very important even if the patient appears well.
General advice for the future
Most children with major heart disease cannot manage as much physical exercise as other children. We do not usually stop children with heart disease from doing exercise, as they usually know best themselves when to stop and rest, but it is probably best to avoid really hard exercise and competitive sport, although it is important to be active to maintain health.
All patients with pulmonary atresia and VSD will be at risk of infection in the heart (called endocarditis), both before and after surgery. Such infections may be caused by infections of the teeth or gums. It is important to visit the dentist regularly and to remind the dentist at each visit of the heart abnormality. Ear or body piercing and tattooing are best avoided as they also carry a small risk of infection which may spread to the heart.
