Adult
- About
- Meet The Team
- Conditions
- Anticoagulation in Pregnancy
- Aortic Dilatation and Pregnancy
- Aortic Valve Disease
- Aortic Valve Replacement
- Atrial Septal Defect
- Coarctation - Transcatheter stent (keyhole) treatment
- Coarctation of the Aorta
- Congenitally Corrected Transposition of the Great Arteries
- Ebsteins Anomaly
- Eisenmenger’s Syndrome
- Fontan Circulation
- Mitral Valve Repair/Replacement
- Normal Heart
- Patent Foramen Ovale
- Pregnancy information for women with metal heart valves
- Pulmonary Incompetence
- Pulmonary Stenosis
- Pulmonary Valve Replacement - Surgery
- Pulmonary valve replacement - Transcatheter (keyhole) treatment
- Repaired Atrioventricular Septal Defects
- Sub-aortic Stenosis
- Surgical treatment of Atrial Septal Defect
- Tetralogy of Fallot
- Transposition of the Great Arteries - The Atrial Switch (Mustard or Senning) procedure
- Transposition of the Great Arteries – Arterial Switch
- Ventricular Septal Defect
- Ventricular Septal Defect - Transcatheter (keyhole) treatment
- Patient Feedback
- Making the most of your clinic appointment
- Your Appointment in Outpatients
- Easy Read Guide for Out Patients
- Cardiac Catheter
- Transoesophageal Echocardiogram
- MRI
- Surgery & "Top Tips" for coming into hospital
- Lifestyle Advice
- Exercise
- Heart Failure
- End of Life and Palliative Care
- Looking after your oral health
- Dentists Information Section: Dental care in adults at risk of Infective Endocarditis
- Yorkshire Regional Genetic Service
- Support
- Video Diaries
- Second Opinion
- Monitoring Results at Leeds Infirmary
- Professionals
Surgical treatment of Atrial Septal Defect
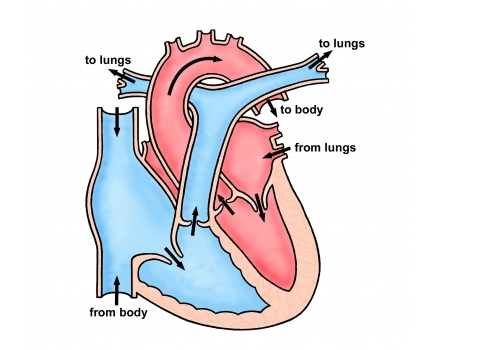
An atrial septal defect (or “ASD”) is a hole between the two smaller pumping chambers of the heart. It allows blood to cross from the left chamber to the right leading to extra flow through the lung artery. Usually patients with ASD’s have very few symptoms but eventually, during later adult life breathlessness and electrical instability of the heart can develop.
There are three types of ASD’s:
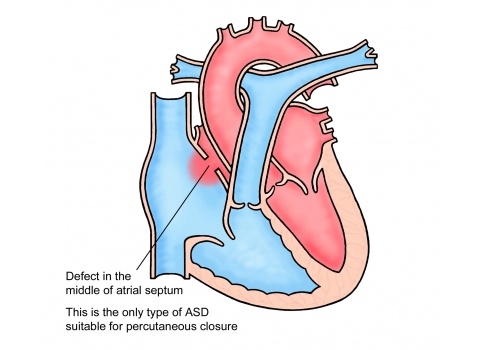
Secundum ASD. This is the most common ASD, affecting around 90% of people with ASD’s. It is caused when part of the atrial septum does not close whilst the heart is developing. This results in a hole in the middle of the wall separating the two atria.
Sinus Venosus ASD. This defect occurs in the part of the atrial septum close to where a large vein enters the heart. As a result, the drainage of one or more veins may be abnormal in that the veins drain into the right atrium, rather than the left atrium.
Primum ASD. This defect occurs in the lower part of the atrial septum and often is associated with mitral and tricuspid heart valve problems.
Will my defect need closing?
We would generally recommend closure of all but the smallest of ASD’s, unless other problems are present that would make this unwise (for example damage to the lungs, which can occur in some patients with ASD’s). Your cardiologist will make an assessment of the hole in your heart and discuss treatment with you. If the best treatment option for you is surgery then you will meet the surgeon and nurse specialist in outpatients before your operation.
The Operation
ASDs were among the first heart abnormalities to be treated with an operation in the 1950’s. The operation is always performed under general anaesthetic so you will be asleep. The surgeon makes an opening in the middle of the chest through the breast bone to get to the heart. During the operation, the function of the heart
and lungs is taken over by a machine (heart bypass). The surgeon can then stop the heart and stitch the hole closed or cover it with a patch. After the operation the breastbone is closed using stainless steel wires and surgical drains (tubes) are positioned in the chest to allow any excess fluid to drain. As a precaution, pacing wires that can be used to help the heart rate are placed on the surface of the heart – these are removed 4-5 days after the operation. The chest drains are usually removed within 2-3 days.
The procedure is safe with a risk of dying of around 1 in 300. There is an even smaller risk of brain damage (stroke) related to the use of the heart bypass machine. Other minor problems can occur, such as bleeding, infection, fluid collecting around the heart or temporary electrical instability but these are rarely serious. After surgery, a short stay on the intensive care unit (usually 1-2 days) and then a period in hospital for observation (usually about 5-7 days) is required before going home. Opening the front of the chest leads to a scar and the chest wall will be sore whilst it heals. The time taken to get fully back to normal varies from person to person but can be up to 3 months.
After the Operation
After your operation you will be closely monitored by both the surgeon and cardiologist. A nurse specialist will visit you on the ward and provide you with a rehabilitation booklet. They will also give you advice about the period after discharge and answer any questions that you may have. The nurse will phone you at home in the week following discharge to check on your progress. You will be given a telephone number that you can contact should you have any concerns between discharge and follow-up. The team’s physiotherapist can provide exercise plans. These are useful as it is important for your recovery to remain active after the operation.
Final Points
In the 2 weeks leading up to your surgery, you will receive an appointment to come to attend preadmission clinic. This is to make sure that you are fit for surgery and also to give you an opportunity to find out more about coming into hospital and ask any questions you may have.
It is important to make sure that all dental work has been completed within 6 months prior to your surgery. This is to prevent possible infections from the mouth causing infection in the heart (endocarditis).
You may need to take some medication following the operation but this is usually temporary (around 6 weeks).
You will need between 6 and 12 weeks off work, depending on your job.
You cannot drive for 6 weeks following the operation.
Once you are fully recovered from the operation you can lead a completely normal life with no restrictions.
