Adult
- About
- Meet The Team
- Conditions
- Anticoagulation in Pregnancy
- Aortic Dilatation and Pregnancy
- Aortic Valve Disease
- Aortic Valve Replacement
- Atrial Septal Defect
- Coarctation - Transcatheter stent (keyhole) treatment
- Coarctation of the Aorta
- Congenitally Corrected Transposition of the Great Arteries
- Ebsteins Anomaly
- Eisenmenger’s Syndrome
- Fontan Circulation
- Mitral Valve Repair/Replacement
- Normal Heart
- Patent Foramen Ovale
- Pregnancy information for women with metal heart valves
- Pulmonary Incompetence
- Pulmonary Stenosis
- Pulmonary Valve Replacement - Surgery
- Pulmonary valve replacement - Transcatheter (keyhole) treatment
- Repaired Atrioventricular Septal Defects
- Sub-aortic Stenosis
- Surgical treatment of Atrial Septal Defect
- Tetralogy of Fallot
- Transposition of the Great Arteries - The Atrial Switch (Mustard or Senning) procedure
- Transposition of the Great Arteries – Arterial Switch
- Ventricular Septal Defect
- Ventricular Septal Defect - Transcatheter (keyhole) treatment
- Patient Feedback
- Making the most of your clinic appointment
- Your Appointment in Outpatients
- Easy Read Guide for Out Patients
- Cardiac Catheter
- Transoesophageal Echocardiogram
- MRI
- Surgery & "Top Tips" for coming into hospital
- Lifestyle Advice
- Exercise
- Heart Failure
- End of Life and Palliative Care
- Looking after your oral health
- Dentists Information Section: Dental care in adults at risk of Infective Endocarditis
- Yorkshire Regional Genetic Service
- Support
- Video Diaries
- Second Opinion
- Monitoring Results at Leeds Infirmary
- Professionals
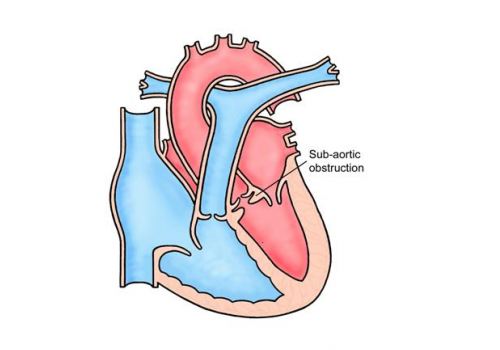
Sub-aortic Stenosis
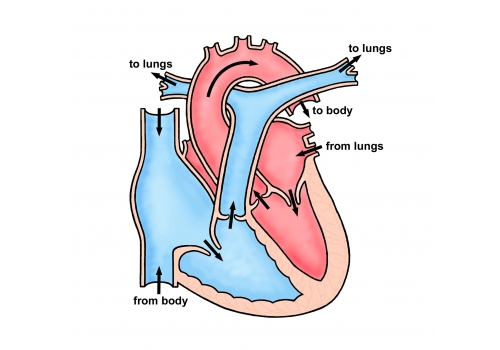
The main pumping chamber of the heart, the left ventricle, pumps blood to the body through a large artery called the aorta. Between the left ventricle and the aorta is a one-way valve, the aortic valve, that prevents blood coming back into the heart once it has been pumped out.
In subaortic stenosis there is excessive growth of tissue just below the aortic valve which causes a narrowing and obstructs blood flowing out of the heart. A severe narrowing is a serious, sometimes even life-threatening, heart condition because the heart has to work very hard to pump blood to the body.
The degree of narrowing can progress over time and so it is important that patients with subaortic stenosis, even if mild, are monitored regularly by a cardiologist. Some patients may have other abnormalities of the heart, including a leaking aortic valve, which will also need to be watched as time goes by.
Tests
Usually a simple ultrasound scan (an echo) is all that is necessary to make the diagnosis. An ECG (an electrical recording of the heart’s activity) can also be helpful.
Treatment
If the narrowing is severe, open heart surgery may be necessary to remove the excess tissue. This can be a challenging operation. It is usually possible to significantly improve the narrowing, but it is not usually possible to remove it completely. Valves, including the aortic valve, can be damaged during the surgery. The tissue that is removed at surgery can grow back over time, so it is important that patients with subaortic stenosis continue to to be monitored regularly in outpatients.
All heart operations carry some risk of death or major complications such as permanent brain damage, kidney damage or pneumonia. For subaortic stenosis the risk of dying at operation is small (about 1 in 100) and the risk of brain damage is also small (around 1 in 100). There is also a small risk (around 1 in 50) of the heart’s electrical system being damaged; if this happens the heart rate will be much slower than normal and a further procedure will be required to implant a pacemaker to make the heart beat faster.
Most patients are in hospital for about a week after their operation, although it may be longer than this if there are complications. It takes approximately 2-3 months to fully recover from open-heart surgery.
Important points to consider
- Exercise: Regular exercise, to a moderate level, is encouraged. It is good for overall health. Activities such as walking, cycling, and swimming are ideal and it is important to warm up and cool down slowly. It is best to avoid really intense cardiovascular exercise, for example distance running, or sudden ‘bursts’ of strenuous activity. Heavy weight lifting should be avoided, but it is usually okay to do low level weights at the gym (up to 15kg), ensuring that you are able to do 3 sets of 12-15 repetitions without any strain/breath-holding. Other activities that cause you to hold your breath or strain to lift/move objects, for example shovelling snow, trying to push a heavy object or playing some brass/woodwind instruments should be avoided as these can raise your blood pressure too much.
- Remember it’s important to come for your review appointments
- Look after your teeth. Good dental hygiene and regular dental checks every 6-12 months are recommended. This is to prevent infection in the heart (endocarditis)
- Due to the increased risk of infection (endocarditis) we also advise against body piercing and tattoos.
- Talk to us before you get pregnant. This is to enable the cardiologist to assess your heart in more detail prior to pregnancy and to arrange further tests if necessary.
- The chances of having a baby born with congenital heart disease are slightly increased from the general population if you have congenital heart disease yourself. The risk is generally quoted as being about 2-4%, compared to 1% for the general population. Your cardiologist can discuss this with you in clinic prior to planning a family. We can offer a specialised scan of your unborn baby’s heart at 18-20 weeks, which can detect any major abnormality of the heart.
Written by the Adult Congenital Team
